Table of Contents
ToggleWhat is Cervical Cancer, Symptoms and Treatment
Contents
What is Cervical Cancer?
What is the cervix?
What are the Causes of Cervical Cancer?
What are the Types of Cervical Cancer?
What are the Symptoms of Cervical Cancer?
What are Cervical Cancer Risk Factors?
What are the Prevention Methods from Cervical Cancer?
Cervical Cancer Stages
Cervical Cancer Vaccine
How is Cervical Cancer Diagnosed?
What is a smear test?
How Is Cervical Cancer Treated?
What is HPV and how is it transmitted?
Genital wart treatment
Frequently Asked Questions About Cervical Cancer
WHAT IS CANCER OF THE ORAL OF THE cervix (cervix)?
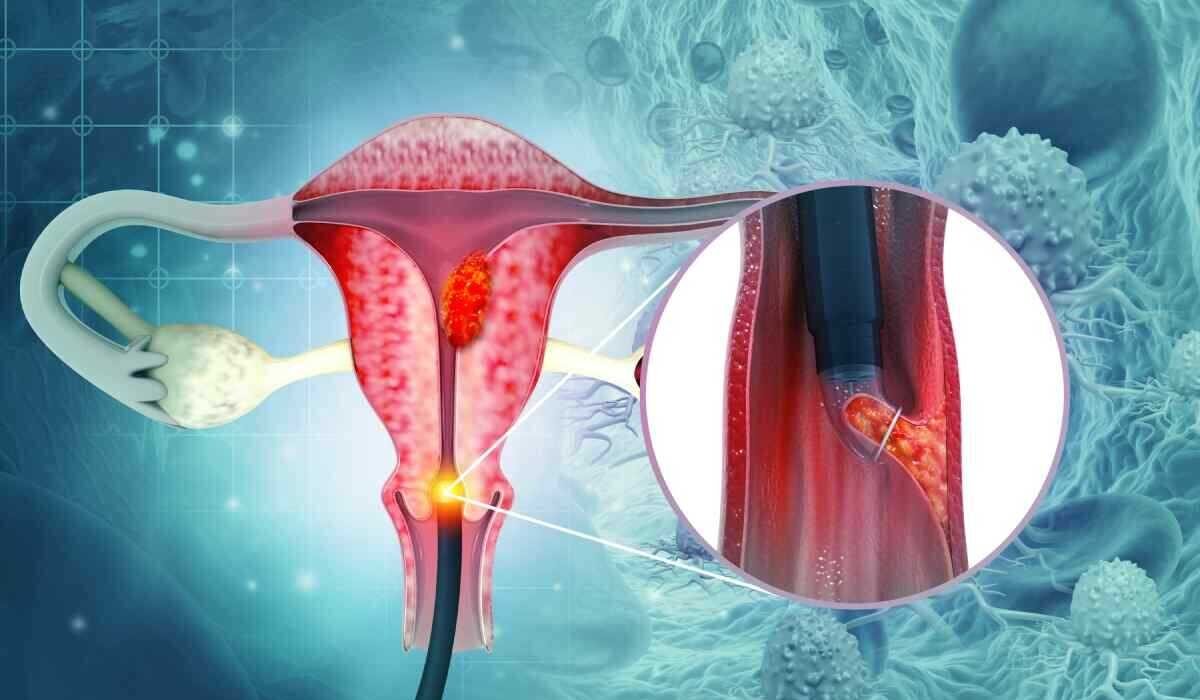
Cervical cancer is the most common gynecological cancer in developing and underdeveloped countries. Every year, 500,000 new cases of uterine cancer are diagnosed worldwide. Cervical cancer, which usually occurs around the age of 50, has also started to be seen in young women in recent years.
The HPV (“Human Papilloma Viruses”) virus, which is responsible for almost all cervical cancers, does not show many symptoms and is highly contagious. Most women defeat the HPV virus they encounter at some point in their lives with the help of their own body defense system. Some HPV viruses come out of this defense system strong and can cause cervical cancer. Taking precautions to prevent the HPV virus that causes the disease and having regular health checks and screenings helps to detect the disease before it occurs or in the early stages of the disease and to be successful in the treatment.
WHAT IS CERVIX?
The cervix, which is the lower part of the uterus, connects the uterus and vagina. As the cervix, the cervix plays an important role in allowing fluids to pass between the uterus and vagina. It also allows the baby to pass through the vagina and leave the uterus during delivery.
WHAT ARE THE CAUSES OF ORAL CANCER?
Like many cancers, the exact cause of cervical cancer is unknown. Only certain factors can facilitate the formation of cervical cancer and accelerate the disease process. In general, the risk factors for cervical cancer are as follows;
to be polygamous
Starting sexual intercourse before the age of 20
To smoke
Weak immune system.
Frequent viral and bacterial infections in genital organs
giving birth to many
Having a low socioeconomic level
Vitamin C and Vitamin A deficiency
WHAT ARE THE TYPES OF CERVICAL CANCER?
Adenocarcinoma
There are different types of cervical cancer. Many types of cervical cancer can be encountered, such as adenocarcinoma and invasive cancers such as squamous cell carcinoma. Among cervical cancers, adenocarcinoma is a relatively aggressive type of cancer that is more difficult to detect and less common. Adenocarcinomas usually form in the inner canal of the cervix, rather than on the outer surface of the cervix. Smear tests use cell samples on the outer surface. Therefore, when the diagnosis of adenocarcinoma is made, the cancer is usually in an advanced stage. More adenocarcinomas occur with HPV types such as 16, 18, 45 and 31 that cause cancer.
WHAT ARE THE SYMPTOMS OF CERVIX CANCER?
Symptoms of cervical cancer may not manifest itself in the early stages. Even in the gynecological examination, the problem in the cervix may not be seen. After the high-risk HPV screening test, which is the cervical cancer screening test, is positive, or abnormalities are detected in the vaginal swab called the smear test, changes can be noticed with instruments that enlarge the cervix called “colposcope”, and the definitive diagnosis can be made with a biopsy taken from the suspicious area.
Symptoms of cervical cancer occur more often in the advanced stages of the disease. Symptoms such as bloody discharge, bleeding after sexual intercourse and irregular menstrual bleeding are among the symptoms of cervical cancer. In advanced cases, the tumor can be noticed even during examination. As cervical cancer progresses, urinary problems, defecation difficulties and leg pain may occur.
One of the symptoms of cervical cancer, bleeding that occurs unexpectedly immediately after sexual intercourse or the next day is called “postcoital bleeding”. Postcoital bleeding is an important finding and may be an early sign of cervical cancer.
Genital warts caused by HPV are not considered a sign of cervical cancer. Because some types of HPV cause genital warts, while some types cause changes in the cells of the cervix in women. However, due to the fact that genital warts are noticed and possible high-risk HPV types may be present, a detailed examination and HPV typing must be done. A cervical swab is taken to find out if the person has HPV infection. According to the results of the examination, whether there is an HPV infection and if there is, the type can be determined.
If cervical cancer has progressed to advanced stages, its symptoms can be summarized as follows;
Urine and stool leakage from the vagina
Back pain
leg pain
Loss of appetite
pelvic pain
swollen feet
weight loss
Fatigue, weakness
Bone pain and fractures
WHAT ARE THE RISK FACTORS OF CERVICAL CANCER?
Causes of cervical cancer include multiple births, having sexual intercourse at an early age, having multiple partners and smoking. HPV infection has been observed in 98% of cervical cancer patients. There are more than a hundred types of HPV, which is usually transmitted by sexual intercourse. In particular, types 16 and 18 cause cervical cancer, while types 6 and 11 cause warts on the genital organs.
Conditions such as polygamy, sexual intercourse before the age of 20, smoking, weak immune system, frequent viral and bacterial infections in genital organs, multiple births, low socioeconomic level, vitamin C and vitamin A deficiency are among the risk factors for cervical cancer. is counted.
WHAT ARE THE METHODS OF PROTECTION FROM uterine mouth cancer?
Cervical cancer prevention methods can be listed as follows:
Have regular doctor checkups
Get HPV vaccines
Avoid cigarettes and tobacco products
strengthen the immune system
Be wary of sexually transmitted diseases
eat healthy
Take precautions against obesity
PHASES OF CANCER OF THE CERVICE
The process leading to cervical cancer proceeds as cervical cancer after CIN 1, CIN 2, CIN 3. In the first stage, 70-90%, 40-45% in the second stage, and 30-35% in the third stage, spontaneous regression can be seen in the disease. In patients who do not receive any treatment, the disease turns into advanced cancer over years. In the early stages, there is no need to remove the uterus, and complete recovery can be achieved by partially removing the cervix with simple surgical procedures called LEEP, conization. These patients may become pregnant and have a baby after treatment.
Cervical cancer stages can be listed as follows;
Stage 0: The abnormal cells are in the innermost layer of the cervix. It is also called carcinoma insutu.
Stage I: Cancer cells are found only in the cervix. Tumor size can vary between 3 mm and 4 cm.
Stage II A: The cancer has spread beyond the cervix to the upper two-thirds of the vagina, but has not spread to the tissues around the uterus.
Stage II B: The cancer has spread beyond the cervix to the upper two-thirds of the vagina and the tissues around the uterus.
Stage III A: The cancer has spread to the lower part of the vagina but not to the pelvic wall.
Stage IIIB: The cancer has spread to the pelvic wall or has invaded the ureters, the tubes through which the kidneys connect to the bladder, obstructing the passage of urine and causing enlargement of the kidneys.
Stage IV: The cancer has spread outside the cervix to the bladder, rectum, or other parts of the body.
CERVIX CANCER VACCINE
Sexually transmitted HPV can cause cervical cancer. To protect against HPV, it is recommended that girls and boys and adults between the ages of 9 and 26 should be vaccinated against cervical cancer. Although 3 vaccines (9, 4 and 2 vaccines) have received FDA approval and are being used in the USA, the 9 vaccine has still not arrived in our country. The double vaccine contains virus-like particles of HPV types 16 and 18, which are the most common cause of cervical tumors, and provides immunity against these types, while the quadruple vaccine also contains virus-like particles of HPV types 6 and 11, which cause warts, in addition to these types. It also protects against warts. The latest vaccines, the 9-vaccine, contain virus-like particles of 31, 33, 45, 52 and 58 in other high-risk HPV types in addition to HPV types 6,11,16,18 in the 4-vaccine and cervical It provides a higher level of protection as it provides immunity against more HPV types that cause cancer. These vaccines also provide some immunity against other HPV types by cross-reaction.
For children aged 9 to 15 years, 2 doses of the vaccine are sufficient. There should be an interval of 6-12 months between the first and second doses of vaccines. For the 15-26 age group, 3 doses of vaccine are recommended at 0, 1 and 6 months. Since the probability of encountering HPV after the age of 26 is high, vaccination is not recommended, but it can be done in appropriate cases by discussing this issue with the physician. HPV vaccine is administered intramuscularly. It can be applied from the shoulder or hip.
Getting the cervical cancer vaccine without ever encountering HPV can prevent most cases of cervical cancer. It is protective in cancers of the vagina and vulva as well as cervical cancer. Types 4 and 9 vaccines can prevent genital warts and anal cancers in men and women. Since some types of HPV are also linked to cancers that develop in the mouth and throat, they also provide protection against these cancers. CDC (The Centers for Disease Control and Prevention) recommends routine HPV vaccination to girls and boys after the age of 9. The ideal vaccination time for the cervical cancer vaccine is the period before sexual experience begins, that is, before contact with the HPV virus. When HPV is infected, the vaccine may not be as effective as the recommended time.
HOW IS CERVICAL ORAL CANCER DIAGNOSED?
The diagnosis of cervical cancer can be made by gynecological examination in the advanced stage, and by colposcopic examination and biopsies performed as a result of detection of positivity in the high-risk HPV DNA test, which are screening tests, or an abnormality in the smear test, in the early stage. In cervical cancer, whose success rate is 80-85% when caught and treated at an early stage, biopsy is also very important for the diagnosis of the disease and for an accurate treatment plan.
The first step in cervical cancer is to diagnose cancer and determine the stage of the cancer. For this reason, a biopsy is taken from the cervix and cancer staging is done. Cervical cancer staging is defined by the spread of the cancer in the body. Staging is based on pelvic and rectal examination in addition to radiological work and other possible diagnostic tests. Apart from smear and biopsy, these tests are used in the diagnosis of cervical cancer;
WHAT IS THE SMEAR TEST?
The smear test is an extremely simple and painless cancer screening method. It is very important for women to have a smear test to prevent cervical cancer. The smear test is done in two ways. In the classical method; The discharge taken is smeared on a glass and sent to the laboratory after it is detected with a special spray. In the second way; The material taken is poured into a special liquid in a bottle. In this way, it is sent to the laboratory, where it passes through certain stages and undergoes a microscopic examination.
All women over the age of 21 who have started an active sexual life should have a smear test. If active sexual life has started before this age, smear test is recommended within the first three years from the starting age. In patients with normal smear test, if there is no other risk factor, it is sufficient to perform a test every 3 years. Tests should not be interrupted during menopause either. After the age of 65, if the patient has at least three normal smear test results by that time, smear tests can be terminated with the knowledge of his doctor. In addition, if a suspicious situation is observed in the smear test, the test can be performed at more frequent intervals or further examination can be applied.
Colposcopy: It is the magnifying examination of the epithelium lining the cervix by looking at the cervix with a special instrument similar to a binocular. Cervical cancer is not something that starts in a day. The deterioration that begins in cells increases over time and gradually. It is possible to follow these changes by seeing them with colposcope examination. If the colposcopy examination is evaluated together with the smear, the error rate decreases significantly.
These tests are also used in the diagnosis and staging of cervical cancer.
Rectovaginal examination; In this test, the breech and vaginal area are examined simultaneously. It is a simple pelvic exam that can be done in office conditions. It is understood whether the cancer has spread beyond the cervix.
CT scan; A CT scan, also called a computed tomography, begins with an intravenous injection of a radiopaque substance. This substance provides better visualization of internal organs in x-rays.
MRI (Magnetic Resonance Imaging) scan; This test uses magnetic radio waves and a computer to image internal organs and tissues.
PET (Positron Emission Tomography) scan; Radioactive glucose is injected into the vein, and the areas of the body where glucose is used at a high rate are determined in PET. Cancer cells are more active than normal cells and use more glucose. Cancer cells appear brighter in this test.
In addition, a chest X-ray and blood count may be requested to determine the spread of cancer to the breast or lungs.
HOW IS CANCER OF THE uterine cervix treated?
Genital warts caused by HPV virus infection can be treated by burning, freezing, surgery or with the help of local creams. The disappearance of the wart as a result of this treatment does not mean that it will not appear again. In some people, the wart does not recur after treatment; In some, wart formation can be observed at frequent intervals. The treatment should be repeated in each new wart formation. The risk of recurrence of genital warts depends on how strong the immune system is. It is known that in HPV virus infections, without treatment, the person can spontaneously remove the virus from his body.
In the treatment of cervical cancer, surgical intervention, radiotherapy and chemotherapy methods are used alone or in combination with each other. If the pre-cancerous lesion (CIN 2-3) has not penetrated deep into the tissue, the area it holds in the cervix can be determined by colposcopy. With the surgical removal of the area, the area that can become cancerous is eliminated, and a high rate of recovery is achieved in the patient. With a simple surgical procedure, the patient can be discharged on the same day. If the cancer has become invasive, that is, deep into the tissue, there are two treatment options. In this case, “radical hysterectomy”, which is an extensive and difficult operation that will take a long time, is performed. At the same time, because cancer cells occupy the lymph nodes in the pelvic area, they are also removed. The alternative is chemo-radiotherapy; The cancer cells in that area are sensitized to the radiation with chemotherapy drug, then radiotherapy is applied to the patient and the follow-up is continued. If it is in the late stage, chemotherapy is given, but the recovery rate in these patients is very low.
WHAT IS HPV, HOW IS IT TRANSMITTED?
HPV is a sexually transmitted virus that can cause cervical cancer. HPV (Human papilloma virus), which is seen in more than 95% of women diagnosed with cervical cancer, is a virus that infects the genital area and spreads by contact. It causes warts in the genital area, especially in women, and cancer in the cervix, external genitalia and reproductive tract. The HPV virus is very insidious and can continue to spread for months without showing any symptoms. Situations in which symptoms of the virus appear several months or years after infection are called “silent infections”.
HPV virus can cause genital warts in men and women, cervical cancer in women, and penile cancer in men. HPV, an infection that should be taken seriously, can be controlled by the immune system of some people. It should not be forgotten that a virus that cannot be inactivated by the immune system can continue to exist for years without showing any symptoms. Without any complaints, a person can carry the infection for years. This does not prevent the spread of the disease, and the virus can continue to be transmitted during intercourse.
HPV virus types are divided into risk groups according to the probability of causing cervical cancer. Types that cause more warts are in the low-risk group for cervical cancer. Therefore, it is not a case that every genital wart will turn into cervical cancer.
GENITAL WARTS TREATMENT
Warts caused by HPV virus infection; It can be treated by burning, freezing, surgery or with the help of local creams. The disappearance of the genital wart as a result of this treatment does not mean that it will not appear again. In some people, genital warts do not recur after treatment; In some, genital wart formation can be observed at frequent intervals. Treatment should be repeated in each new genital wart formation. It is known that in HPV virus infections, without treatment, the person can spontaneously remove the virus from his body.
Cervical cancer after treatment
Depending on the stage of the cancer and the type of treatment, cervical cancer may not go away or reappear after treatment. A new cancer may also arise in another part of the body. For this reason, routine controls and smear tests are important even after the treatment is over. Your doctor may want you to have more frequent smear tests in the first few years after treatment. This is done to make sure that all cancer cells are destroyed. Other tests and procedures may also be required. Your doctor will work with you to plan the check-ups you need, even after treatment is over.
FREQUENTLY ASKED QUESTIONS ABOUT CANCER OF THE UTILITY
Is Cervical Cancer Contagious?
The biggest factor causing cervical cancer is HPV. This virus was detected in 99.7% of the patients. Although cervical cancer is not contagious, HPV is the most common sexually transmitted virus. After sexual contact with people with warts in the genital area, there is a high rate of contagiousness, such as 60%.
HPV is mostly sexually transmitted; At very low rates, it can be transmitted by hand contact, toilet and personal hygiene materials. Multiple partners are at high risk for HPV transmission.
What Are the First Symptoms of Cervical Cancer?
Symptoms such as bloody discharge, bleeding after sexual intercourse and irregular menstrual bleeding can be seen among the first signs of cervical cancer.
Where Does Uterine Cancer Pain Hit?
Cervical cancer may present with symptoms such as back pain, leg pain, pelvic pain, bone pain. In addition, pain and pressure sensation in the lower abdomen, pain during sexual intercourse, and weight loss can also be seen.
Can Cervical Cancer be felt by hand?
During palpation, the doctor places two fingers inside the vagina and the other hand on the lower abdomen. In this way, organs and any palpable mass can be felt.
At What Stage Does Uterine Cancer Show Symptoms?
Symptoms of cervical cancer appear in the advanced stages of the disease. Tumor can be seen during examination in advanced stages. As cervical cancer progresses, urinary problems, difficulty in defecation, and leg pain can be seen.
At What Age Does Cervical Cancer Start?
Cervical cancer, which usually occurs during menopause around the age of 50, has recently been seen in young women. Although breast cancer ranks first among the most common cancers in women, cervical cancer can prevent breast cancer due to its life-threatening feature.
What Happens in the Smear Test? Is Cervical Cancer Obvious?
The smear test is performed to detect changes that may occur in the vagina before it turns into cancer. In this way, women can easily have the opportunity to be treated before they reach the stage of cancer. Women may need to have a smear test in the routine determined by obstetricians.